Jump to: Results | Summary
Abstract
Acute Myeloid Leukemia (AML) is a devastating hematological malignancy with a global incidence of approximately 120,000 new cases annually and a five-year survival rate below 30%. Despite advances in therpeutic strategies. treatment outcomes remain poor. The complexity of AML, characterized by genetic heterogeneity and clonal evolution, presents significant challenges for the development and testing of novel therapeutics in clinically relevant settings.
AML research relies heavily on cell lines and syngeneic models, or immunodeficient models without an added human immune system component. While these systems provide valuable insights, they fail to fully recapitulate the genetic and phenotypic diversity of primary human AML tumors. Traditional models often lack the tumor microenvironment and immune interactions critical for therapeutic evaluation. Furthermore, existing models generally rely on extensively passaged samples, which lose the heterogeneity and clonal diversity intrinsic to AML, undermining their clinical relevance.
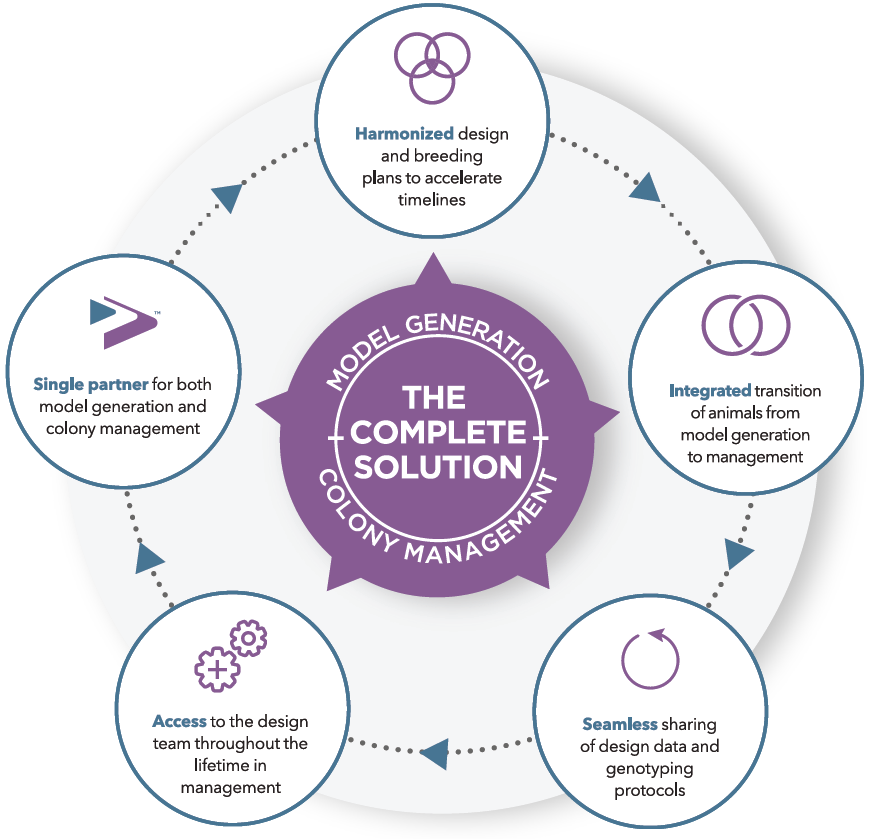
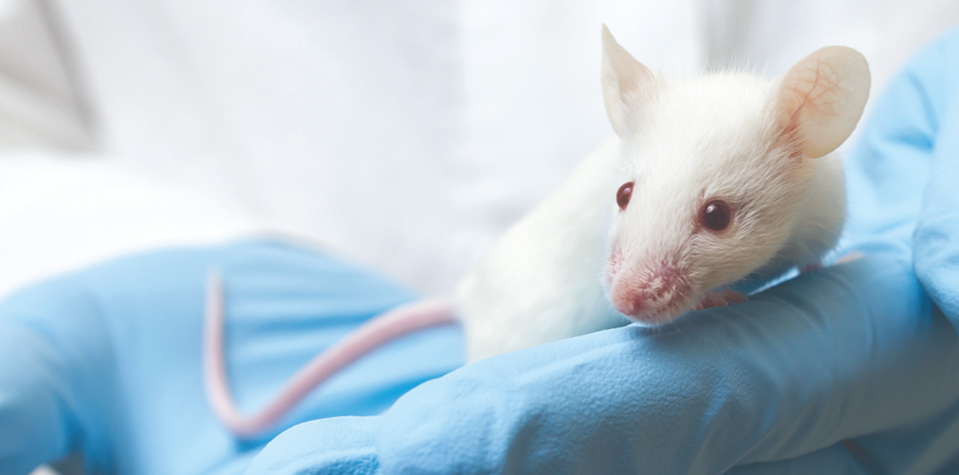
To address these limitations, we developed an in vivo AML platform using human CD34+ engrafted NOG-EXL mice. NOG-EXL was selected as the preferred in vivo model as it has been successfully engrafted with primary AML PDXs, albeit not also with a humanized immune system component. This novel platform was built on a bank of over 50 patient-derived AML models that have been passaged, preserving their native tumor characteristics. Humanized NOG-EXL mice, transgenic for human IL-3 and GM-CSF, were used to promote primary AML engraftment as well as CD34+ stem cell differentiation into a wider repertoire of human myeloid and lymphoid lineages. The models are fully characterized with RNA sequencing, proteomics, diagnostic data, and detailed clinical histories. By retaining the complexity and clonal architecture of primary AML tumors, these models provide a truly translational system for preclinical drug testing.
AML donors were evaluated in humanized NOG-EXL. CD34+ engraftment was confirmed in humanized NOG-EXL mice followed by engraftment with AML primary cells. Human immune cell engraftment and AML cancer progression were assessed at different timepoints through flow cytometry on peripheral blood and bone marrow. A custom flow cytometry panel was used to identify the human immune cells present as well as the main AML sub-populations including the AML progenitors, AML blasts and monoblasts.
This novel approach bridges a critical gap in AML research by offering a robust, clinically relevant platform that reflects real-world disease biology. It demonstrates an in vivo model with primary never-passed AML PDX in the context of a human immune system. The Champions AML humanized model sets a new standard for preclinical evaluation, promising to accelerate the development of personalized therapies and improve outcomes for AML patients worldwide.
Materials & Methods
Primary AML samples: Sourced from Champions Oncology’s AML tumor bank, featuring over 50 fully characterized patient-derived models maintaining in a neverpassaged state to preserve heterogeneity and clonal evolution these models truly represent the patients in the clinic. Target expression, mutational profile, proteomics, and clinical histories have been used for model selection.
Humanized NOG-EXL Mice: NOG mice transgenic for human IL-3 and GM-CSF (NOG-EXL) were used as these support not only high levels of CD34+ engraftment with resulting myeloid and lymphoid differentiation but also a high success rate in primary AML engraftment and growth. NOG-EXL mice engrafted with human CD34+ hematopoietic stem cells (HSCs) were provided by Taconic Biosciences. HSC donors were selected based on HLA matching to specific AML tumors and HSC engraftment was confirmed by flow cytometry by Taconic Biosciences.
AML Progression & Immune Profiling: Custom flow cytometry panel used to track AML blasts, monoblasts, and AML progenitors and human immune cell subpopulations have been developed ensuring proper engraftment in peripheral blood and bone marrow at different time points. CD34+ Donors and AML Donors were specifically mismatched on one HLA criteria in order to differentiate healthy donor and diseased AML myeloid cells by flow cytometry.










.jpg)

.jpg)
.jpg)
.jpg)
.jpg)


.jpg)


.jpg)
.jpg)


.jpg)




.jpg)

.jpg)










