 The field of immuno-oncology continues to grow and its focus now includes various therapeutic approaches modulating one or more human immune cell types. T cells have been the most widely investigated and are the target of a spectrum of biologics; examples include manipulation of native T cells by checkpoint inhibitors and adoptive cell therapies such as CAR-T cells or the ex vivo expansion of TILs. The FDA has approved multiple checkpoint inhibitor drugs (e.g., targeting PD-1, PD-L1, or CTLA4), some of which have become the standard of care in certain clinical circumstances. More recently, cell therapies have also been given FDA approval, and researchers are taking these successes in T cell targeting to branch out beyond to other cell types, namely to promising NK cell approaches.
The field of immuno-oncology continues to grow and its focus now includes various therapeutic approaches modulating one or more human immune cell types. T cells have been the most widely investigated and are the target of a spectrum of biologics; examples include manipulation of native T cells by checkpoint inhibitors and adoptive cell therapies such as CAR-T cells or the ex vivo expansion of TILs. The FDA has approved multiple checkpoint inhibitor drugs (e.g., targeting PD-1, PD-L1, or CTLA4), some of which have become the standard of care in certain clinical circumstances. More recently, cell therapies have also been given FDA approval, and researchers are taking these successes in T cell targeting to branch out beyond to other cell types, namely to promising NK cell approaches.
NK Cells in Immuno-Oncology
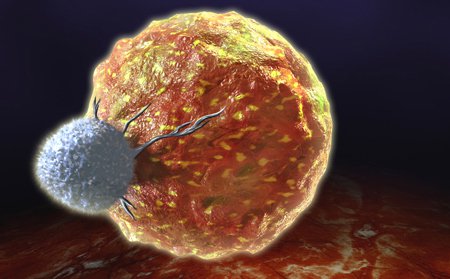
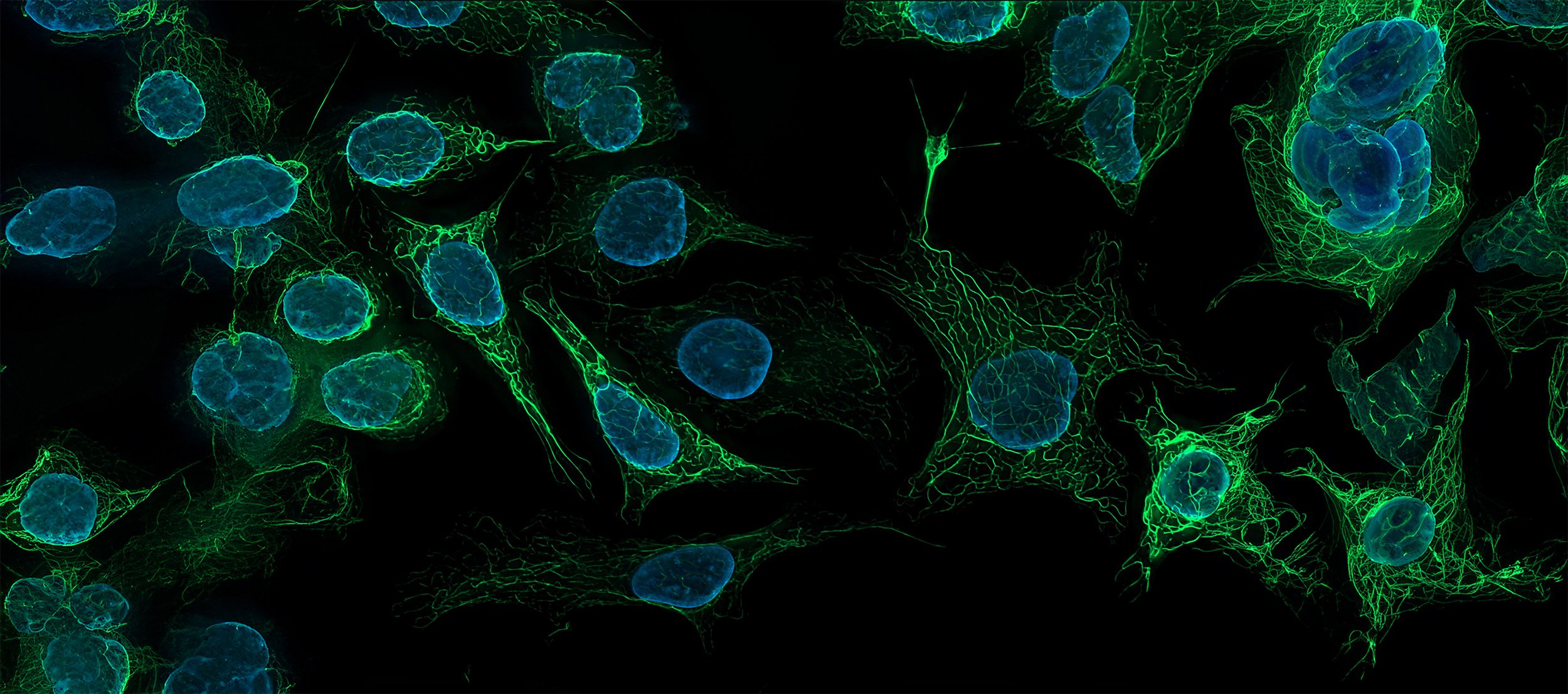
Natural Killer (NK) cells are large lymphocytes that can kill tumor or virally-infected cells via several mechanisms. NK cells have an essential role in tumor surveillance1 and thus remain relevant targets for immunotherapy since the earliest use of monoclonal antibodies (mAb) to treat cancer. While mAb drugs can directly kill tumor cells, they also engage/recruit aspects of the patient's immune system in their efficacy. Many mAb drugs (the majority of which are immunoglobulin G) work through an NK cell-mediated antibody-dependent cellular cytotoxicity (ADCC) mechanism. Thus, ADCC is a critical mechanism of action exploited for immuno-oncology drug discovery and clinical efficacy.Awakening a Natural Killer
Tumors can escape immune surveillance by NK and other immune cells, and some immunotherapy approaches are designed to break down this common tumor defense mechanism. Antibody engineering is generating new drug classes such as bispecific or multispecific engagers, which can target both tumor antigens as well as immune cell receptors. With the binding of two distinct targets (one on the tumor the other on an immune cell capable of a kill function), these therapeutics concentrate activated immune cells into close proximity with tumor cells, reducing the ability of the tumor to evade detection and destruction. These new drug classes can target various immune cell types; those that target NK cells are sometimes called NK cell engagers (NKCE), bispecific killer cell engagers (BiKEs), or trispecific killer cell engagers (TriKEs). Examples include Innate Pharma's NKp46-based NK cell engager IPH6101/SAR443579 and Affimed's bispecific antibody AFM24 which target the EGFR tumor antigen.These drugs can be used alone or in combination with adoptive NK cell therapy to increase the number of viable, active NK cells present in a patient. For example, NKMax America has an enhanced NK cell technology that involves ex vivo expansion and activation of autologous or allogeneic NK cells, which Affimed is trialing in combination with AFM24. Affimed recently announced positive preclinical results both on AFM24 monotherapy and in combination with adoptive NK cells at the 2021 American Association for Cancer Research (AACR) meeting.
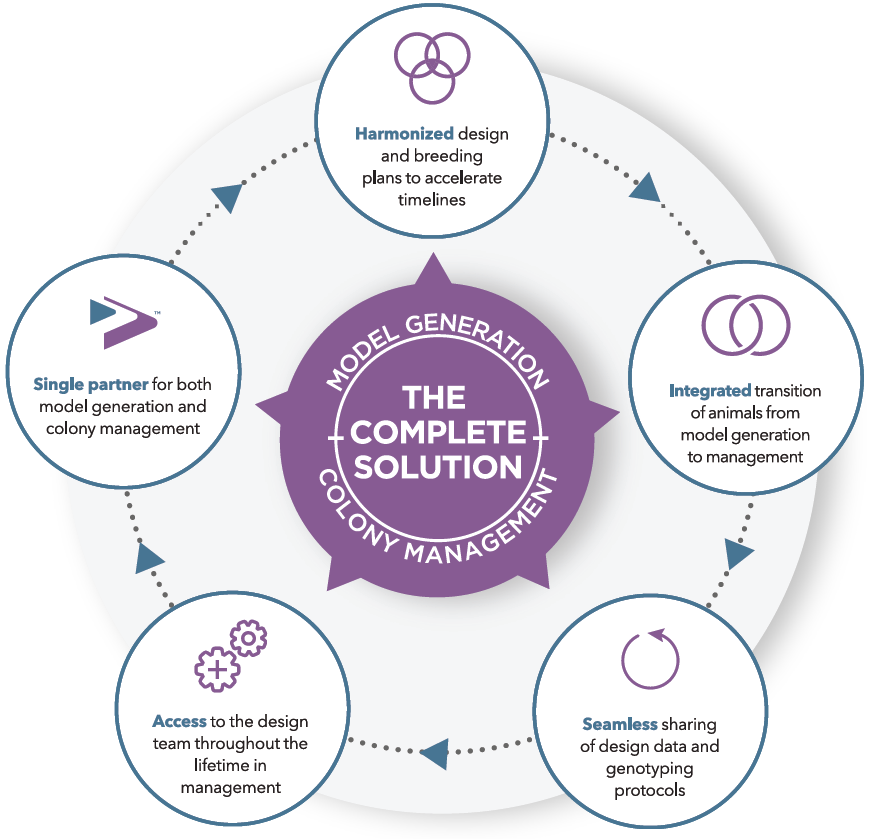
Modeling Human NK cells in a Preclinical Setting with hIL-15 NOG Mice
Intellia Therapeutics used NK-engrafted hIL-15 NOG mice to develop an in vivo NK cytotoxicity assay. hIL-15 NOG mice were engrafted with primary human NK cells. Four weeks later, luciferase-labeled K562 human chronic myelogenous leukemia cells were injected. hIL-15 NOG mice engrafted with NK cells were able to rapidly eliminate injected tumor cells, and little to no tumor growth was observed 24 days post-tumor injection, as measured through whole body bioluminescence imaging. In control hIL-15 NOG mice which were not engrafted with NK cells, tumor cells were readily observed via bioluminescence after injection, and tumor growth was well established in multiple sites 24 days later. This represents a useful model for in vivo efficacy evaluation of adoptive cell therapies2.Another strategy under evaluation is combination therapy consisting of adoptive NK cell transfer along with a drug designed to increase the anti-tumor activity of NK cells. To evaluate the efficacy of NK cell-engaging molecule AFM24 in combination with NK cell transfer in an in vivo preclinical setting, Affimed employed a xenograft model with Taconic's hIL-15 NOG mice, which support superior engraftment and persistence of human NK cells. Expression of human IL-15 is required for persistence of human NK cells in mice; without this, engrafted NK cells disappear within one to two weeks in NOG mice which do not express a consistent plasma concentration of that supportive cytokine. hIL-15 NOG mice were inoculated with a luciferase-labeled, EGFR-expressing human breast cancer cell line. Mice were dosed repeatedly with either:
- Vehicle
- human NK cells + a vehicle
- human NK cells + a negative control
- human NK cells + co-administered AFM24 at two different doses
- human NK cells pre-loaded with AFM24
CARrying Onward
NK cells engineered to express chimeric antigen receptors (CARs), also called CAR-NK cells, can be generated from autologous or allogeneic NK cells which are isolated, engineered to express the CAR, expanded ex vivo, and then infused into a patient. A number of clinical trials are ongoing for CAR-NK therapies, but so far none have been approved by the FDA. Allogeneic cells for use in CAR-NK cell development can be taken from healthy donors, such as sourcing NK cells from adult peripheral blood or umbilical cord blood.Fate Therapeutics has taken another approach to adoptive NK cell therapy by generating NK cells, which in some cases are further genetically modified, from master inducible pluripotent stem cell (iPSC) lines. An advantage of this method is that therapies are essentially off-the-shelf, rather than having to be developed specifically for each patient. However, starting from master iPSCs means that all transplants are allogeneic, which can pose challenges from a pharmacokinetic standpoint. Fate's engineered NK cell products incorporate a range of modifications, from CD38 knockout or expression of an IL-15 fusion receptor, which promote NK cell persistence, to the introduction of CARs designed to target tumor antigens. Cell therapies with multiple modifications are quite intriguing, but more straightforward methods are also being explored.










.jpg)

.jpg)
.jpg)
.jpg)
.jpg)


.jpg)


.jpg)
.jpg)


.jpg)



.jpg)

.jpg)





