 Even in the era of COVID-19, scientific research beyond the scope of novel infectious diseases marches on. Such was the case recently for the virtual 23rd annual American Society for Gene & Cell Therapy (ASGCT) meeting. ASGCT convenes the clinical and research communities and patient advocates annually to advance knowledge, awareness, and education leading to discovery and clinical application of gene and cell therapies to alleviate disease.
Even in the era of COVID-19, scientific research beyond the scope of novel infectious diseases marches on. Such was the case recently for the virtual 23rd annual American Society for Gene & Cell Therapy (ASGCT) meeting. ASGCT convenes the clinical and research communities and patient advocates annually to advance knowledge, awareness, and education leading to discovery and clinical application of gene and cell therapies to alleviate disease. Oncology is a prominent focus at recent ASGCT meetings. Cellular therapies for cancer aim to improve the immune system's ability to fight the tumor and represent a paradigm shift in oncology therapy over the last decade. In adoptive cell therapy, also referred to as cellular immunotherapy, immune cells from either the patient or a healthy donor are isolated, sometimes genetically engineered to improve their ability to target tumors, expanded and returned to the patient. These cells recognize and contribute to tumor elimination and may be used as a monotherapy or in combination with other treatments. Additionally, bone marrow or cell transplantation is a therapeutic option for many hematological malignancies.
Types of Cell Therapy for Cancer
According to Cancer Cell Therapies: The Clinical Trial Landscape1 published by Nature Reviews in March, 2020, all aspects of the cancer cell therapy pipeline had a year over year increase in 2020 compared to 2019 (Figure 1).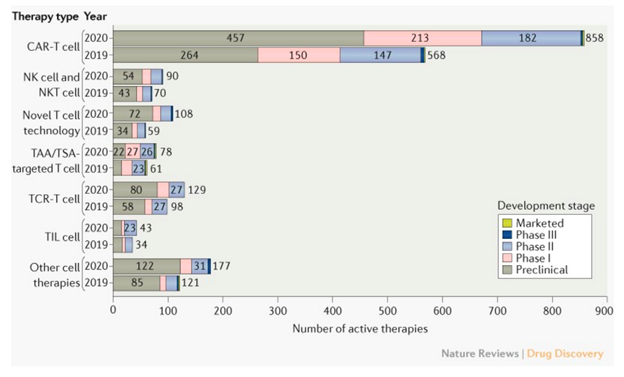
Figure 1: Trends in the cancer cell therapy pipeline, comparing March 2020 to March 2019. TAA: tumor-associated antigen; TCR: T cell receptor; TIL: tumor-infiltrating lymphocyte; TSA: tumor-specific antigen. From Yu et al1.
Major classifications of cell therapies for cancer include CAR-T (chimeric antigen receptor T cells), TCR (T cell receptor), TIL (tumor infiltrating leukocytes), and NK (natural killer) cells. As depicted in Figure 1, T cells play a pivotal role in cellular immunotherapy approaches against cancer. Strategies focused on the T cell receptor (TCR) specifically, which utilizes innate T cell mechanisms to recognize cancer-specific antigens and therefore attack the cancer, have emerged as an attractive therapeutic alternative to CAR-T approaches1.Confounds of GvHD in Cancer Cell Therapy — Role of T cells
Graft versus host disease (GvHD) is a potentially life-threatening immune-related side effect of stem cell, bone marrow, or other allogeneic (i.e., non-autologous) cell therapies where immune cells in the transplant graft attack cells or tissues in the host. Complications of GvHD must be considered for any allogeneic cell-based immunotherapy for cancer. GvHD remains a significant concern for cell-based therapies, despite optimizations to the donor-host matching process and cell transplantation methods2. Immunocompetent graft-derived T cells are mechanistically implicated in GvHD and the host tissues most acutely involved in GvHD include skin, gastrointestinal tract, and liver. Symptoms of GvHD include skin rash, weight loss, and jaundice, and severe GvHD can be life-threatening3.Improved Mouse Models to Study GvHD
Preclinical models are necessary to study mechanisms of cell-based immunotherapies for cancer, including potential adverse effects of GvHD. Intellia Therapeutics presented data at ASGCT 2020 related to T cell-mediated mechanisms of GvHD in a mouse model of xenogeneic GvHD utilizing human peripheral blood mononuclear (hPBMC) cells engrafted in Taconic Biosciences' super immunocompromised NOG mice (Figure 2).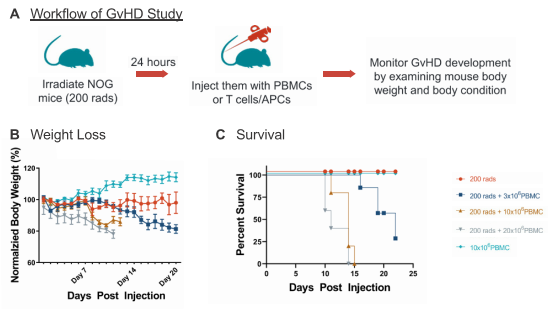
Figure 2: Establishment of an in vivo GvHD model. To induce xenogeneic GvHD in NOG models, the mice were irradiated with 200 rads prior to inoculation with donor PBMC in varying amounts (A). Body weight (B) and survival rate (C) were determined over the course of the study.
Using this mouse model of GvHD, Intellia showed that T cell receptors (TCRs) are required for GvHD in the hPBMC-engrafted NOG mice (Figure 3). Specifically, NOG mice co-injected with human antigen presenting cells (APCs) and wild type human T cells were moribund within 3 weeks; however, 80% survival out to 90 days was observed in mice receiving APCs in addition to T cells in which TCR function was ablated due to loss of TCR α chain via knockout of the TRAC locus.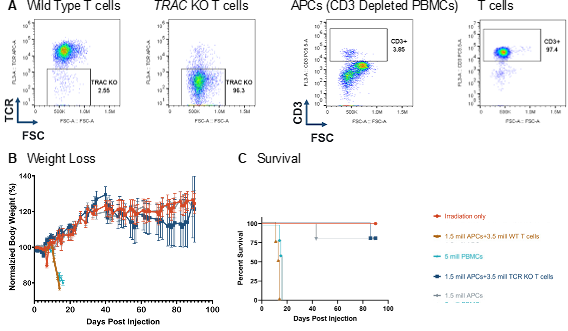
Figure 3: TCR KO T cells did not induce GvHD. (A) The endogenous TCR was removed via CRISPR/Cas9 targeting of the TRAC locus with 97% efficiency. (B) Injection of TCR KO T cells in to NOG mice did not induce GvHD, as no mice lost >20% of body weight, as compared to baseline (B) and induce similar survival as compared to controls (C).
Natural T reg cells can ameliorate GvHD in hPBMC engrafted NOG mice
Intellia also showed that natural T regulatory cells (nTreg) can suppress the deleterious effects of xenogeneic GvHD in NOG mice engrafted with hPBMC (Figure 4). Prolonged survival and attenuated loss of body weight was observed in NOG mice co-injected with human nTregs and hPBMCs, compared to mice transplanted with hPBMCs alone.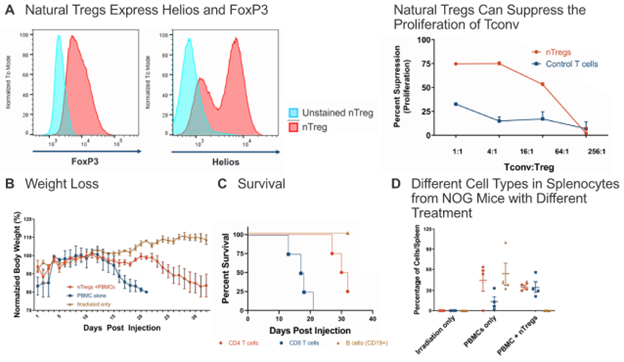
Figure 4: Natural Tregs can suppress GvHD in vivo. (A) Natural Tregs, which express FoxP3 and Helios, were mixed with conventional T cells (Tconv) at various ratios in a mixed lymphocyte reaction and their suppression activity was determined. (B) To test the suppressive effect of nTregs in vivo, NOG mice were irradiated with 200 rads one day prior to engraftment of PBMCs +/- Treg at 1:1. nTreg were able to suppress GvHD, as determined by monitoring body weight loss (B) and prolonged survival (C). nTreg cells suppressed the number of CD19+ B cells in spleen, potentially impacting the slowed onset of GvHD (D).
Advanced preclinical models support present and future immunotherapy studies
The annual ASGCT conference showcased the significant advances in the field of cell therapy for oncology. Specifically, the data presented by Intellia at ASGCT 2020 emphasize the importance of understanding mechanisms of T cell-mediated GvHD, both as a preliminary step in assessing safety and toxicity in developing cell-based immunotherapies, as well as elucidating potential adjunct therapeutic approaches to ameliorate GvHD in diverse applications.As reviewed by Boieri and colleagues, preclinical animal models are fundamental to the understanding of GvHD pathophysiology and enable discovery of novel treatments4. Efforts to optimize preclinical models and tools for oncology remain an active area of research and development, and humanized models are a key tool in that quest.






.jpg)

.jpg)
.jpg)
.jpg)
.jpg)





.jpg)
.jpg)


.jpg)



.jpg)




.jpg)

.jpg)
.jpg)





